Hospitals across the U.S. face heavy financial headwinds as the healthcare industry grapples with a shortage of skilled professionals. Ongoing payer denials, including DRG downgrades, add gasoline to the blazing financial fire. These issues are intensified by the complexities of Clinical Documentation Integrity (CDI), which is crucial for DRG revenue integrity.
Dr. Bilal Mushtaq, Senior Vice President of DRG Revenue Integrity at CorroHealth, states, “Around 2016, Payers shifted to clinical validation over coding validation denials, and the annual changes in coding guidelines each October add to the complexities in Clinical documentation improvement initiatives for both staff and providers.”
Dr. Mushtaq highlights the resulting physician fatigue and the effects of COVID-19 in the healthcare industry, which have led to suboptimal documentation practices and responses like ‘unable to determine.’ These factors considerably affect CDI accuracy, thus impacting DRG and revenue integrity.
The Vital Role of DRGs in Reimbursement Accuracy
Accurate and comprehensive clinical documentation, facilitated by effective CDI practices, is crucial. Properly assigned DRGs accurately reflect a patient’s care complexity and the resources required to provide care.
“When I was working on the clinical team, we started with basic tools like Excel sheets, spending hours filtering data,” Dr. Mushtaq states. “This was time-consuming and prone to errors. With VISION, teams can move to a smarter, high-level approach.”
Advanced technology from CorroHealth simplifies CDI management by streamlining DRG classification. Teams no longer need to manually apply rules thanks to VISION’s code database and algorithms.
Utilizing CMI for Benchmarking
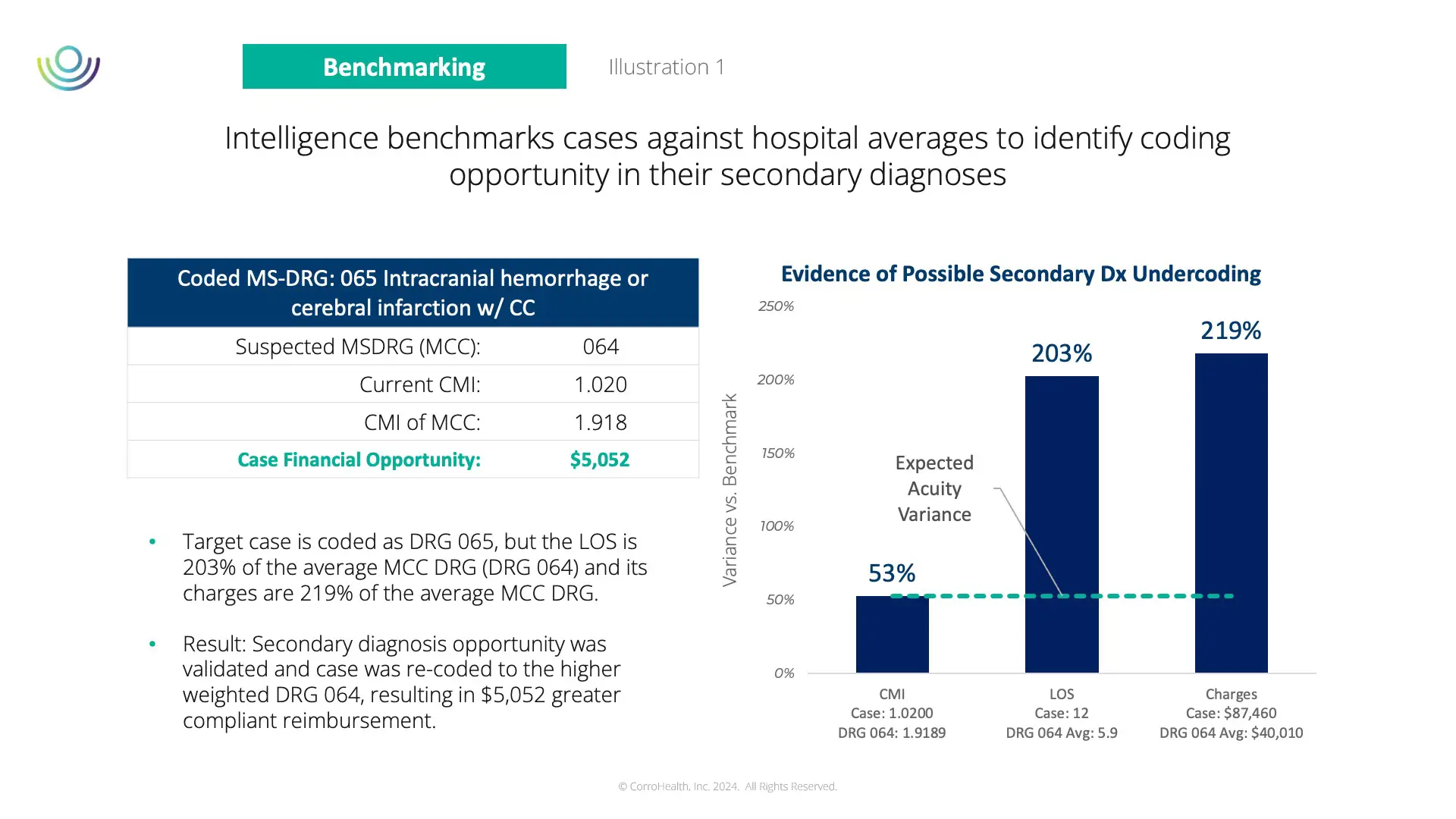
The shift towards more sophisticated tools like VISION is mirrored in using CMI benchmarking, a unique methodology that helps drive VISION to intelligently select, score, and prioritize cases for review.
Incorrect DRG assignments adversely affect the Case Mix Index (CMI), a crucial metric indicating the average severity and resource consumption for a hospital’s patient population. CMI represents the average DRG weight per patient discharge, revealing the complexity and resource needs of a patient’s stay. The synergy between optimized DRGs and an accurate CMI forms the backbone of a financially robust and fair healthcare reimbursement system. Benchmarking CMI facilitates performance comparisons with industry peers and uncovers areas for DRG enhancements.
Dr. Mushtaq highlights CMI’s importance, “Analytics and trends in reporting are crucial, making our focus more intelligent. It allows us to identify outliers in costs and charges and concentrate on specific DRGs.”
For instance, in the example in illustration 1, VISION identified an outlier case coded as DRG 065 with a disproportionate length of stay and charges. VISION’s benchmarking rules led the system to flag this case for expert review. After reclassification to DRG 064, the compliant reimbursement increased to just over $5,000, and the CMI was adjusted accordingly. This demonstrates how CMI benchmarking, integrated into VISION, offers a data-driven approach to refine DRG integrity by highlighting high-potential cases and streamlining CDI efforts.