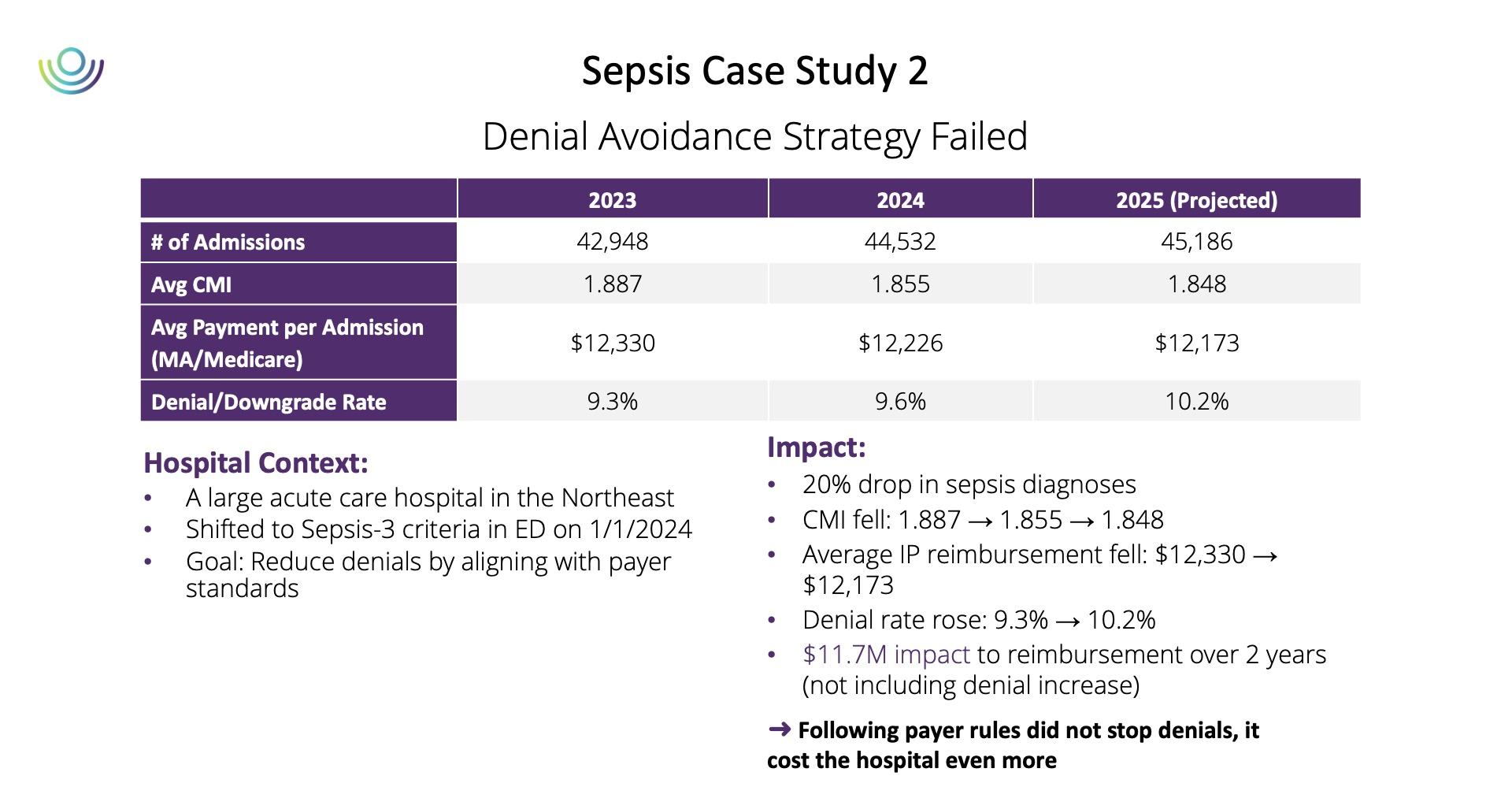
So, what happened? Even though the hospital was following the payers’ criteria every time, a more aggressive attack on high-value MCC’s targeting the ambiguities of the coding and documentation allowed the payers to reimburse at lower rates or not reimburse at all. Sepsis also remained a primary payer target, even when most denied cases met the payers’ own Sepsis3 criteria.
Like Lucy and Charlie Brown, the ball had been pulled, the target had been moved, and the provider lost once again.
Enter AI: What it Adds and What it Doesn’t
Artificial and generative intelligence have flooded healthcare with promises to automate documentation and eliminate administrative burden. In many areas, those tools deliver real results. But as Dr. Jerilyn Morrissey pointed out during a Becker’s Health IT + RCM featured session, AI isn’t a silver bullet for payer denials—and where it’s applied matters.
“Many organizations are rushing to use AI to write appeal letters,” she said. “But that’s like asking the bot at the payer to argue with the bot at your hospital. It’s not a value-add activity.”
Yes, AI can help scale your appeals process—but it’s a volume game. “When written appeals only overturn about 20% of the time,” Morrissey explained, “you have to ask whether producing more letters justifies the cost of the technology.”
The real opportunity for AI lies upstream, before the denial occurs. “Payers have been using AI to generate denials for more than a decade,” Morrissey continued. “That puck has already moved. The real power comes from using clinical AI and GenAI to strengthen documentation accuracy and defensibility before a claim ever reaches the payer.”
AI works best when it supports clinicians — validating documentation, flagging inconsistencies, and helping ensure that diagnoses like sepsis are fully supported with payer-ready evidence. That’s how providers can “skate to where the puck is going,” leveraging AI not just for reaction, but for prevention.
Innovative Approaches to Fighting Denials: Tech + People + Policy
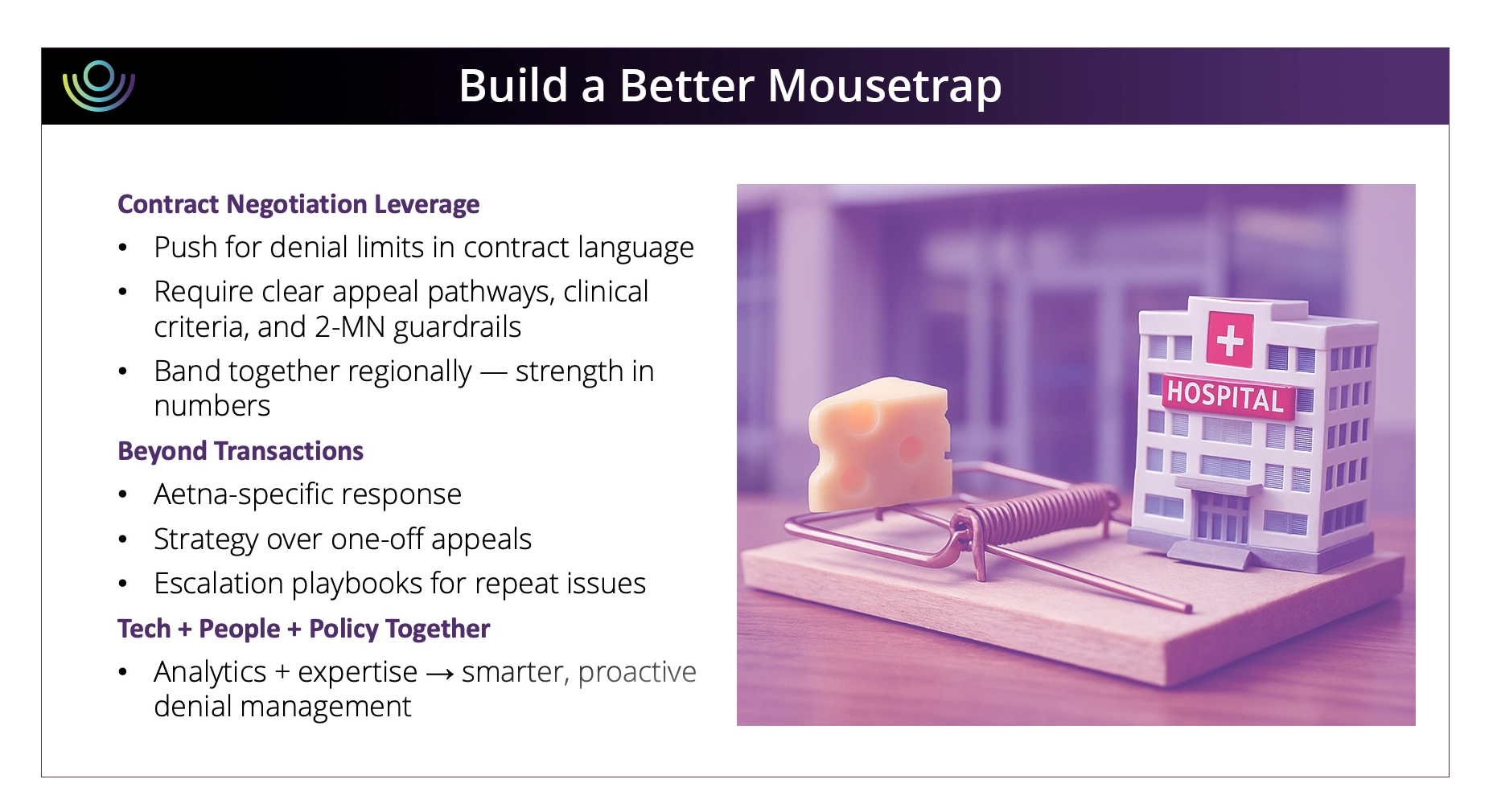
While many hospitals look at their denials management strategy from the standpoint of the value of each type of denial, Dr. Morrissey and Ms. Seippel recommend a more holistic and strategic approach, built on intimate knowledge of regulations and informed by your data. They recommend providers take the following actions:
Get your data straight. Effectively analyzing your data and getting clear on what problems really exist for your hospital is imperative, explains Dr. Morrissey. “I can’t tell you how often I’ve heard a hospital say that they have a huge problem with this, or that. And when we actually run the data, it’s a tiny problem.” Understanding the data, having really robust denials analytics ensures you understand where you need to focus, whether it be on process improvement or on your problematic payers. Some tips: track your approvals, educate everyone who touches a claim, and track denial data by DRG and impact, not just one or the other. Additionally, providers should be wary of self-downgrading to “prevent” denials – not only because data shows it’s an ineffective strategy – but also because it forfeits the hospital’s right to escalate issues later.
Use contract negotiation as a battlefield. Payers generally want to remain in network to preserve member access and the contractual discounts that follow. Leverage emerges only when payers fear losing market share, and that concern creates opportunities to negotiate protective contract language that hospitals have struggled to secure so far. Some smaller facilities have partnered with nearby providers when they lack sufficient individual volume to influence contracts. “There’s power in numbers,” says Seippel. “If one hospital in a region threatens to go out of network, it doesn’t really do a lot. But if all hospitals in the region go out of network, those patients still need care… so use that power.” The intent is never to restrict patient access, but when hospitals coordinate, more protective language tends to get successfully negotiated into agreements.
Integrate your clinical and revenue cycle systems. Working in silos often leads to gaps in documentation and missed revenue opportunities. An example of this, explains Seippel, might be, “make sure that your patient accounting team knows that a payment does not necessarily mean that there isn’t a denial. That no denial on the 835 doesn’t mean you’ve been paid appropriately.” Even instituting simple solutions such as regular cross-functional meetings and increased education on CMS rules and updated payer denial tactics can help seal leaks in your procedures.