OVERVIEW
Northeast Health System is one of the most comprehensive academic health care systems in the country, providing treatment and services to more than three million patients each year. The 11-hospital system resulted from a merger between two health systems.
THE PROBLEM
Northeast Health System embraced a traditional outsourced Physician Advisor model using two different vendors. With the consolidation of the two health systems, one of the priorities was implementing consistent processes across the new organization. The Centers for Medicare and Medicaid Services (CMS) implemented the 2-Midnight Rule to address three vulnerabilities:
- reduce inappropriate short inpatient stays,
- reduce inappropriate long observation stays, and
- reduce variability in decision making regarding admission status.
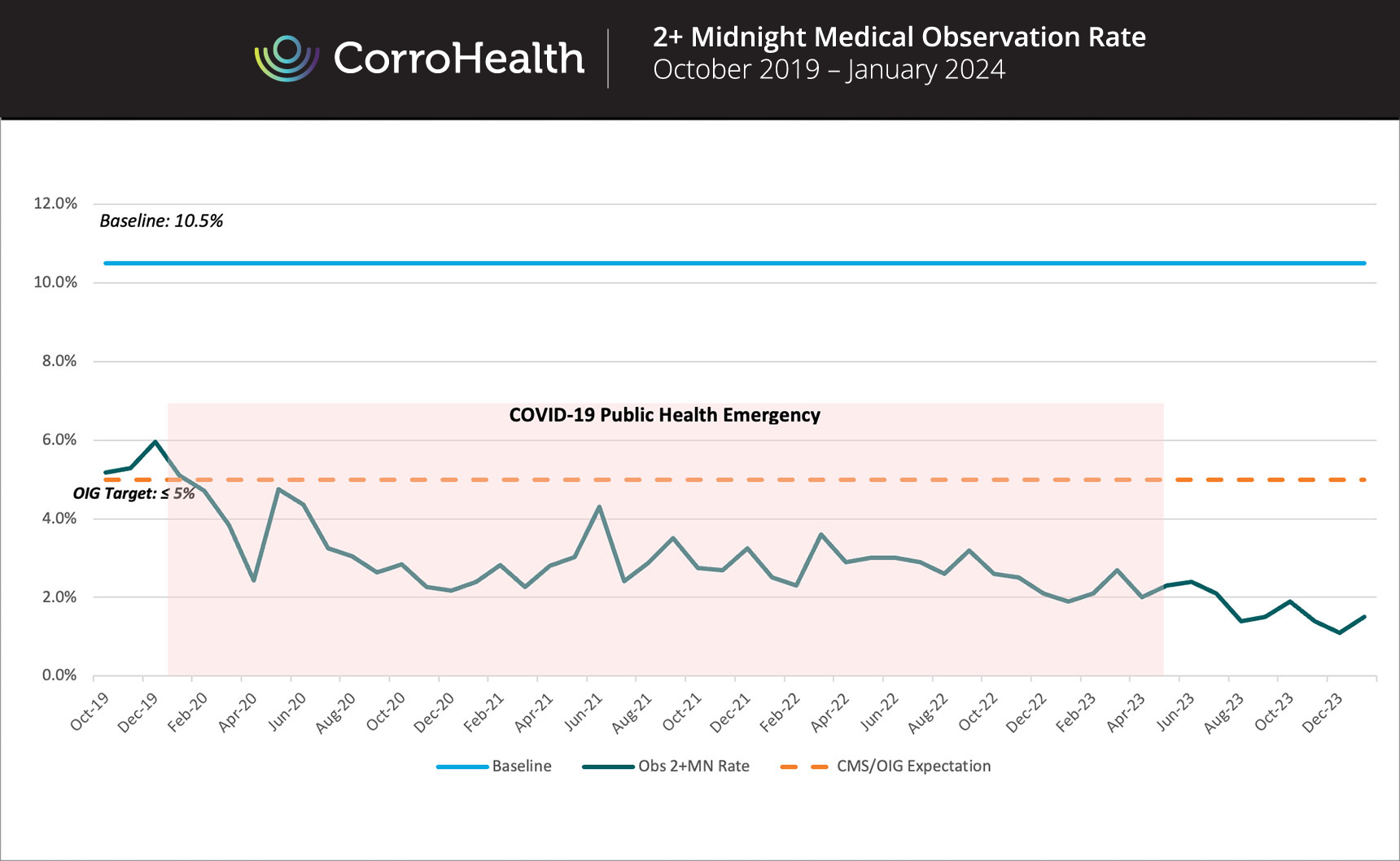
Consistent with CMS objectives, Northeast Health System’s goal was to increase efficiencies, reduce inappropriate observation rates in line with CMS/OIG guidelines, and eliminate the high degree of variability amongst its eleven hospitals in the application of the CMS 2-Midnight Rule for Traditional Medicare-Fee-For-Service (MFFS) patients. The existing vendors’ solutions were not addressing the inappropriately rising observation rates nor the variability of these rates across the facilities.
Not satisfied with either of its two vendors and to ensure best in class compliance and revenue integrity, Northeast Health System leadership engaged CorroHealth.
THE SOLUTION
Northeast Health System partnered with CorroHealth to perform a Clinical Revenue Cycle Opportunity Assessment to assess variability in the application of the CMS 2-Midnight Rule and identify if there was overuse of inappropriate long observation.
After performing the Assessment, CorroHealth showed that implementing a 2-Midnight Rule compliant approach would enable a revenue integrity opportunity of $17 million. This also reduces the statusing variability, and an over usage of the inpatient status for short stay cases. The approach would align the system’s performance with CMS and the Office of Inspector General (OIG) guidelines under the 2-Midnight Rule.
Based on this Assessment, Northeast Health System decided to implement the CorroHealth 2- Midnight Rule Program as a pilot at four facilities in early 2019. After only three months of the pilot, Northeast Health System leadership decided to roll-out the program to the other seven hospitals, given the immediate operational, compliance, and financial improvements.
RESULTS
During the Assessment, CorroHealth identified revenue opportunities and compliance risks for all Northeast Health System sites. CorroHealth then utilized this information to implement targeted process recommendations and workflow modifications for Utilization Management and physician staff.
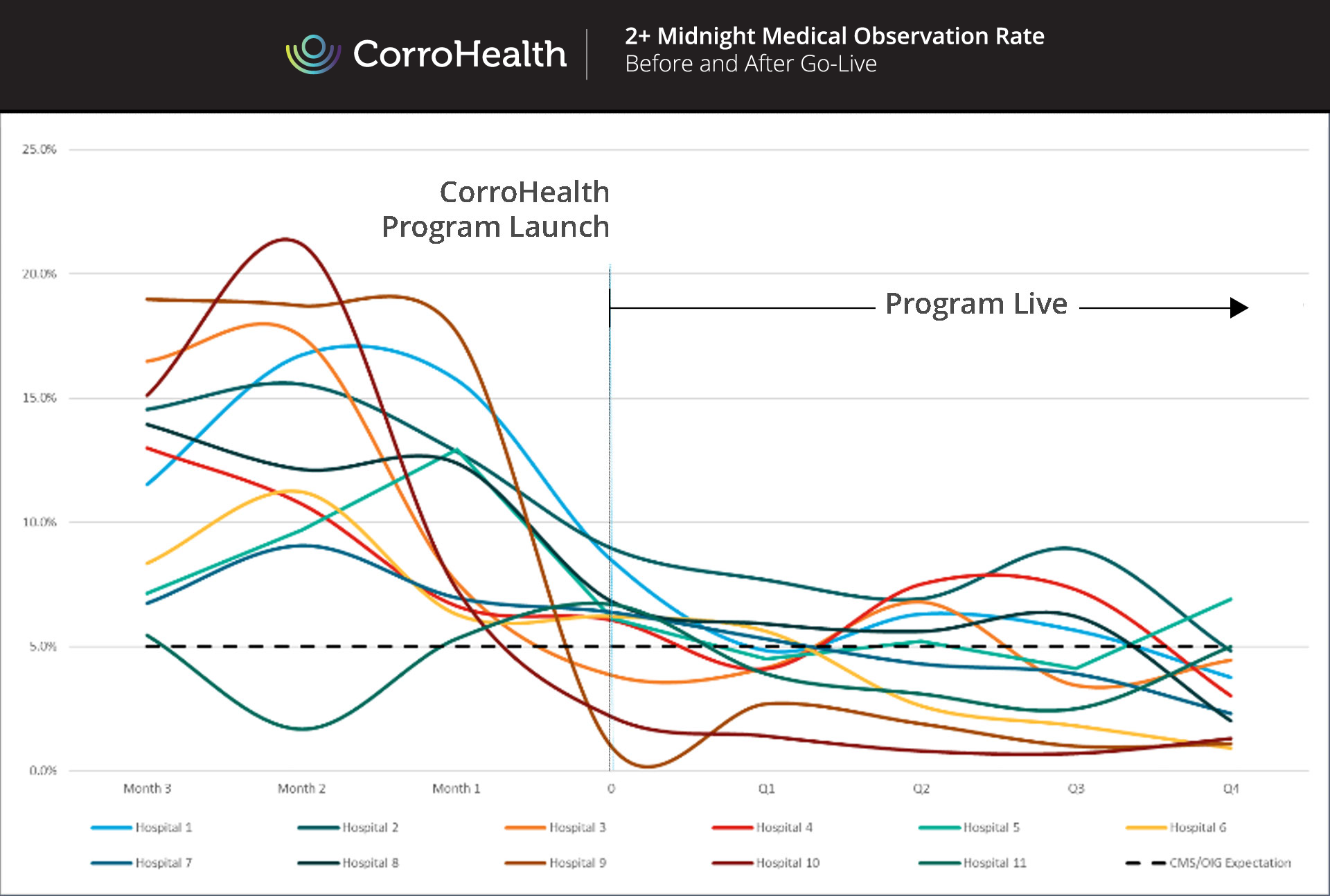
Graph 1 below shows the CorroHealth program’s impact on inappropriate long-stay Observation Rates for every Northeast Health System facility across an eight-month timeframe in 2019.